CAR-T Cell Therapy: A Possible Road to Cancer Remission
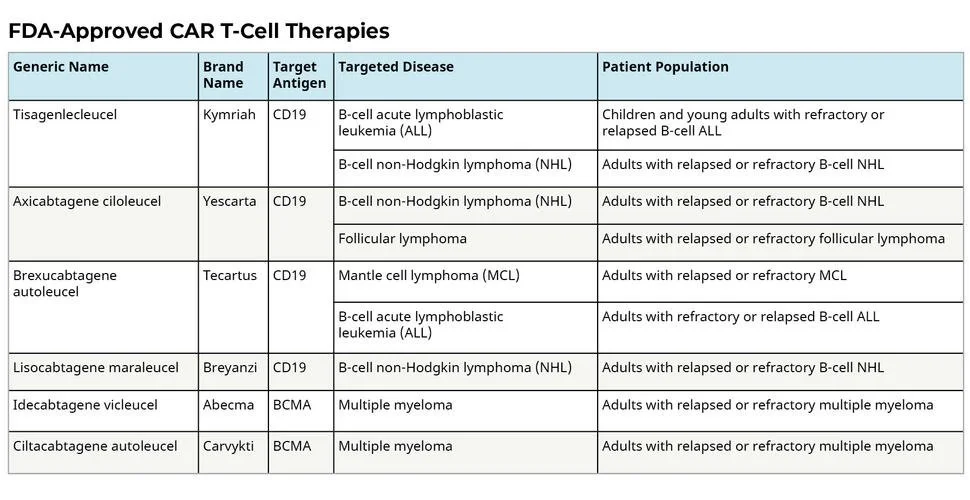
CAR-T cell therapy is a relatively novel treatment for certain types of cancer. The current cancers being treated (with FDA approval) are blood cancers such as pediatric leukemia, non-Hodgkin’s lymphoma, multiple myeloma, etc [1]. The table [2] below shows the FDA-approved CAR-T cell therapies. However, there are several other cancer CAR-T treatments that are currently in the clinical trial phase.
First we will talk about how cancer cells avoid being attacked by the immune system. One way is that these cells will have defects in antigen processing or presentation due to random mutations [3]. Antigens on the surface of a malignant cell is how the immune system recognizes that it is a cancer cell. It is like a logo or a label that broadcasts “I am a cancer cell” to the immune system. So when cancer cells no longer present antigens, the immune system can no longer recognize them. Another mechanism by which cancer cells avoid detection is by a loss of immunogenicity [5]. This essentially means that they will have an increased secretion of suppressive cytokines which essentially tells the immune system that the cancer cell is not a foreign pathogen that needs to be attacked. Another evasion mechanism is these malignant cells will create a local immunosuppressive microenvironment [6] wherein the malignant cancer cells will debilitate any anti-tumor immune responses from the cells surrounding them. This will then prevent the immune system from attacking the malignant cells. Whilst these are some of the most common ways that cancer cells avoid detection, there are many many more evasion mechanisms that they employ.
This problem is being tackled by a field known as cancer immunotherapy. And to begin to understand CAR-T cell therapy, we need to first understand cancer immunotherapy. Cancer immunotherapy relies on the principle of harnessing the body’s own immune system to attack malignant cells [4].
Why is it that the body’s own immune system is the best option for attacking malignant cells? The cancer cells have been able to evade the immune system long enough to grow. So what changes the immune system such that it can now identify the cancer cells?
Cancer immunotherapy, with a focus on answering the question asked above, is a rapidly growing field for several reasons. One big reason is that cancer immunotherapy gives patients the possibility for long-term cancer remission [4] due to our immune systems being able to retain some memory. This means that once a cancer has fully been eliminated, your immune system is likely to remember how to attack it in the future, if the need arises. Another big reason is that cancer immunotherapy may not cause the same potentially harmful side effects as chemotherapy or radiation such as nausea and hair loss. [4.] This is because these traditional cancer treatments also destroy healthy tissues such as the gastrointestinal lining or hair follicles. However, with cancer immunotherapy, you would only target the malignant cells and therefore the treatment should not affect healthy tissues.
CAR-T cell therapy is a type of immunotherapy. The CAR portion stands for Chimeric Antigen Receptor, and these are genetically engineered synthetic receptors on T-cells (taken from the patient’s blood) that can recognize antigens expressed on cancer cells [3]. Once these infused T-cells enter the patient’s body, they will attack the malignant cells, prevent them from growing and eventually eliminate them from the body. The CAR-T cells will remain in the body and will continue to multiply and stay in the body, allowing the immune system to recognize and attack any future malignant cells (thereby offering long term remission).
There are several limitations to CAR-T cell therapy. One possible limitation is a phenomenon known as antigen escape [6] wherein the malignant cells will no longer express the target antigen that the genetically engineered CAR-T cells are targeting. Another limitation is that one of the functions of the T cells (found in the immune system) is to release cytokines, which are little molecules that help to activate the immune response and to direct this response towards a certain area of the body. So when a patient is infused with the CAR-T cells, it results in a huge amount of cytokines flooding the bloodstream, a side effect known as cytokine release syndrome (CRS) [7]. This can cause serious side effects (such as decreased lung function, changes in blood clotting, edema and many others) and in some cases it has a possibility of being fatal. There are also some limitations associated with using CAR-T cells to treat solid tumors and this is primarily due to the tumor’s surrounding immunosuppressive microenvironment which can prevent these engineered T cells from reaching the tumor cells. [6] Additionally, due to tumor heterogeneity (meaning that the antigens on the solid tumors can vary within the patient themselves and between patients), it can be difficult for the CAR-T cells to find an antigen to target [6]. This is a short list of some of the limitations of this new method of cancer treatment but there are several others. However, this is a growing body of research and there are avenues being explored to target these limitations.
CAR-T cell therapy is finally getting its spot in the limelight. This immunotheraputic approach is a key step propelling us forward down the path of developing specialized cancer treatments with as few side effects as possible.
References
CAR T Cell Therapy: Using Immune Cells to Fight Cancer. Pennmedicine.org. (n.d.). Retrieved March 13, 2022, from https://www.pennmedicine.org/cancer/navigating-cancer-care/treatment-types/immunotherapy/what-is-car-t-therapy
Car T cells: Engineering immune cells to treat cancer. National Cancer Institute. (n.d.). Retrieved March 13, 2022, from https://www.cancer.gov/about-cancer/treatment/research/car-t-cells
Squibb, B. M. (n.d.). Car T 101. Lecture. Retrieved March 13, 2022, from https://media.cartcellscience.com/wp-content/uploads/car-t-academy-car-t-101.pdf
Why immunotherapy? Cancer Research Institute. (n.d.). Retrieved March 13, 2022, from https://www.cancerresearch.org/en-us/immunotherapy/why-immunotherapy
Vinay, D. S., Ryan, E. P., Pawelec, G., Talib, W. H., Stagg, J., Elkord, E., Lichtor, T., Decker, W. K., Whelan, R. L., Kumara, H. M. C. S., Signori, E., Honoki, K., Georgakilas, A. G., Amin, A., Helferich, W. G., Boosani, C. S., Guha, G., Ciriolo, M. R., Chen, S., … Kwon, B. S. (2015). Immune evasion in cancer: Mechanistic basis and therapeutic strategies. Seminars in Cancer Biology, 35. https://doi.org/10.1016/j.semcancer.2015.03.004
Sterner, R. C., & Sterner, R. M. (2021). Car-T cell therapy: Current limitations and potential strategies. Blood Cancer Journal, 11(4). https://doi.org/10.1038/s41408-021-00459-7
Car T cells: Engineering immune cells to treat cancer. National Cancer Institute. (n.d.). Retrieved March 13, 2022, from https://www.cancer.gov/about-cancer/treatment/research/car-t-cells